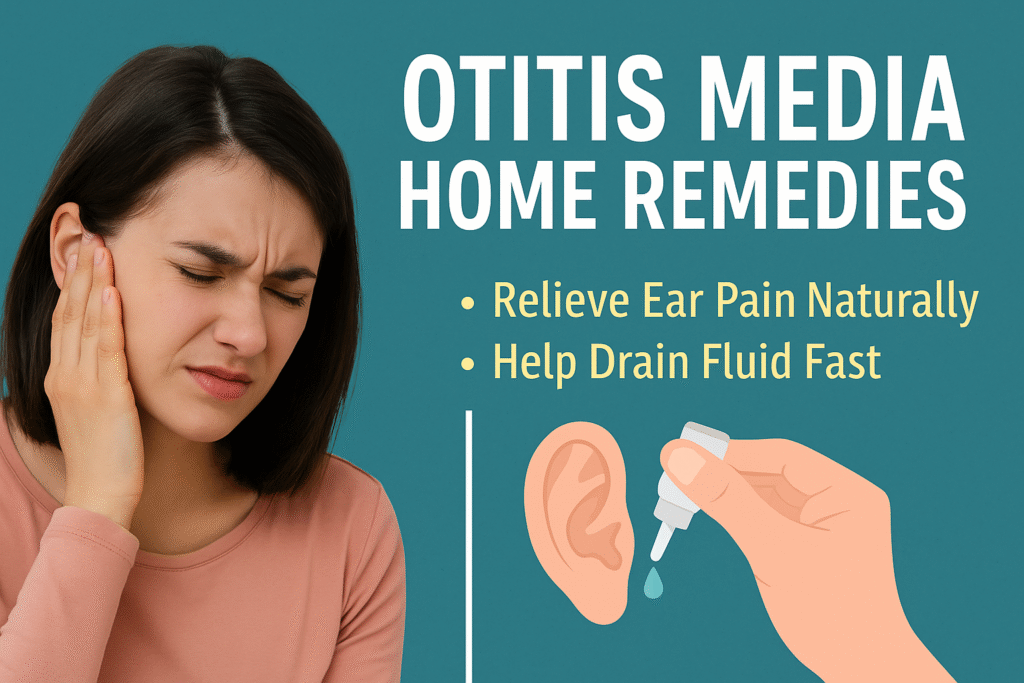
If you’ve ever had that awful ear pain that sticks around no matter what you do, you’re definitely not the only one. Ear infections are super common—especially with kids—and they love to pop up after a cold or a bad allergy episode. In this article, we’re digging into the signs that point to something more than just regular ear discomfort, looking at what actually causes all the inflammation and pressure, and going over current treatments—from simple things you can try at home, to antibiotics, to more long-term fixes if it keeps coming back. Ever had that annoying, slow-building ache in your ear that just keeps nagging at you? Like, maybe it started after a cold—or just decided to show up randomly at night when all you want to do is sleep. That deep, throbbing pain (sometimes with pressure or this weird fullness) could be more than just an annoying earache. Yeah, it might actually be an ear infection. Doctors call it otitis media, and it’s one of those things that hits kids a lot, but adults aren’t totally off the hook either. So here’s the deal: we’re going to talk through the symptoms that should raise an eyebrow, what’s happening in your ear when it gets infected, and what you can do—whether it’s you or your kid dealing with it.

If you’ve ever had that awful ear pain that sticks around no matter what you do, you’re definitely not the only one. Ear infections are super common—especially with kids—and they love to pop up after a cold or a bad allergy episode. In this article, we’re digging into the signs that point to something more than just regular ear discomfort, looking at what actually causes all the inflammation and pressure, and going over current treatments—from simple things you can try at home, to antibiotics, to more long-term fixes if it keeps coming back.
Ever had that annoying, slow-building ache in your ear that just keeps nagging at you? Like, maybe it started after a cold—or just decided to show up randomly at night when all you want to do is sleep. That deep, throbbing pain (sometimes with pressure or this weird fullness) could be more than just an annoying earache. Yeah, it might actually be an ear infection.
Doctors call it otitis media, and it’s one of those things that hits kids a lot, but adults aren’t totally off the hook either. So here’s the deal: we’re going to talk through the symptoms that should raise an eyebrow, what’s happening in your ear when it gets infected, and what you can do—whether it’s you or your kid dealing with it.
Okay, let’s start with the one thing pretty much everyone notices first—ouch, the pain. That sharp, pulsing ear pain that makes you wince or want to clutch your ear like it might fall off. For little kids, it’s often just some crankiness and ear-pulling, which kind of breaks your heart because they can’t always explain why they’re uncomfortable.
Some people say it feels kind of like being underwater, like there’s pressure or fullness inside their ear that won’t ease up. And your hearing can go a little funky too—it might sound like everything’s muffled or like people are speaking from behind a wall. Then there’s the fever, which is really common in kids dealing with this. In more intense cases, you might even see some liquid coming out of the ear, which is, yeah, not great.
Getting a good night’s sleep? Pretty much impossible when your ear feels like it’s being poked with a hundred tiny needles. Super fun.
So here’s what’s going on inside your ear: the infection sets up shop in the little air-filled space behind your eardrum, known as the middle ear. According to the Cleveland Clinic, this usually follows being sick with a cold or having allergy flare-ups.
Basically, when you’re stuffed up or congested—like from a cold or allergies—the Eustachian tube (that tiny channel connecting your throat and middle ear) can get clogged. And when that happens? It traps moisture and gives bacteria or viruses this cozy, warm space to hang out in and multiply, leading straight to inflammation and infection. Great, right?
Kids tend to get hit with these more often, and part of the reason is that their Eustachian tubes just aren’t built for great drainage yet—they’re shorter and more horizontal than adults’. That’s like rolling out the welcome mat for infections. And if you’re someone with allergies? You probably already know the drill: major sinus pressure or congestion can be a solid warning sign that your ears might be next.
These days, treatment isn’t always as aggressive as it used to be. A lot of doctors like to play it by ear (pun sort of intended) and just watch how things go—especially with mild cases, since many of these infections will clear up without doing anything fancy.
In the meantime, though, painkillers like ibuprofen or Tylenol can really take the edge off. And honestly? Holding a warm, cozy compress over your ear feels weirdly soothing—sometimes it’s the simple stuff that helps the most.
Now, if the pain sticks around or gets worse after a few days, that might be the time for antibiotics—especially if a bacterial infection is the culprit. Your doctor will probably peek in your ear with that little flashlight tool (an otoscope) to figure out what’s going on and how to treat it.
And if these infections start feeling like clockwork, especially for kids who seem to catch one every month? That’s when you might hear about preventive strategies—like putting tiny tubes in the eardrums to help with drainage and stop things from building up. It sounds a little scary, but for some families, it’s been a total game changer.

Dealing with stubborn ear pain is the worst, and if it just won’t back off, there’s a good chance an ear infection might be behind it. Getting a feel for the signs, knowing what could be causing it, and figuring out what kind of help you might need—that really can make all the difference. Especially if you’re trying to get back to feeling normal… or at least get some sleep.
Ear Infection (Otitis Media): Symptoms, Causes & Treatment
Ear infection (middle ear) – Symptoms & causes – Mayo Clinic
Ear Infection (Otitis Media) – Johns Hopkins Medicine
Today’s related searches: how to relieve ear pain at home, best home remedies for ear infections, how to use warm compress for earache, when to see a doctor for ear infection, how to use hydrogen peroxide for ear pain, over the counter medicine for ear infection pain, how to help child sleep with ear infection, how to drain fluid from ear naturally, saltwater gargle for ear infection relief, natural remedies for earache in adults
[intro_box]